Teen Suicide Prevention

TEEN SUICIDE CAN BE PREVENTED
This is especially true when those around the teenager who is being affected by depression and anxiety symptoms monitor their loved one for the warning signs. The warning signs include:
- Depression, anxiety, or mood swings.
- Loss of interest in activities that were previously, a lot of fun.
- Withdrawing from friends and family.
- Anxiety, irritability, agitation, aggression, reckless behaviors.
- Sleeplessness or excessive sleeping.
- Self-destructive behavior such as increased drug and alcohol use.
Suicide is now the second leading cause of death for teens and young adults in the United States; a problem that has reached epidemic proportions. The fastest and most efficient way to overcome these types of problems is IV Ketamine therapy.
Suicide does not discriminate among us. People of all genders, ages, economic backgrounds, and ethnicities can be at risk for depression and anxiety. There’s no single cause for these medical conditions.
KNOWING THE WARNING SIGNS AND HOW TO GET HELP CAN SAVE LIVES
The main risk factors for suicide include:
- Depression
- Mental health challenges
- Substance use disorder
- Certain medical conditions
- Chronic pain
- History of prior suicide attempt
- Family history of mental health challenges, substance use, or suicidal behavior
- History of family violence
- Access to unsecured firearms
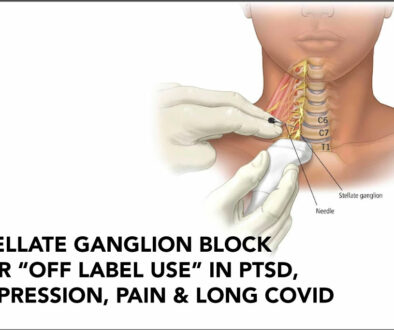
Our clinic has been able to help with all the above situations using IV ketamine therapy. Please investigate this revolutionary therapy that resets the brain and nervous system. Ketamine therapy is the quickest, most accessible therapy to obtain relief from Pain, Depression, Anxiety, PTSD, OCD, ADD, Addictions, Headaches, MS, and Fibromyalgia.
We are one of the most experienced clinics in Kentuckiana [offering Ketamine therapy for 10+ years] and the only one treating teenagers and military Veterans. Veterans are treated at no charge when referred by the VA team. We even treat 12-year-old individuals suffering from the listed conditions which few clinics are comfortable doing.
TESTIMONIALS:
“Best thing I ever did was Ketamine therapy from Dr. Cruz. It was like throwing a light switch. I got my life back.”
Keith Perkins from Clarksville, Indiana
“I tried ketamine to treat my depression. Within a day, I felt relief.”
Alice Levitt Medical Writer and Editor
If you or a loved one is struggling with any of the above situations, please see your doctor, or nurse practitioner, or consider contacting our clinic Kentuckiana Integrative Medicine Kentuckiana Ketamine Institute.
Our Medical Director, Dr. Rafael F. Cruz MD is a medical writer, researcher, and physician educator who has practiced medicine for over 30 years and has helped countless patients with numerous complex health challenges.
Below is another research article demonstrating tremendous benefits in patients suffering from suicidal thinking and bipolar disorder depression.
Ketamine Fast, Effective for Suicidal Crises
Megan Brooks
February 10, 2022
Ketamine is a rapid and effective treatment for suicidal ideation and has a “major” moderating effect based on the primary mental health diagnosis, results of a large randomized controlled trial shows. In addition, a strong effect of ketamine was observed in patients with bipolar disorder, “whereas the effect was moderate and did not quite reach significance in those with other psychiatric disorders and unexpectedly was non-significant in those with major depressive disorders,” the researchers write.
“We assessed for the first time in the same study the effect of ketamine on three a priori defined groups of nonpsychotic patients: those with a bipolar disorder, those with a depressive disorder, and those with other diagnoses,” study investigator Fabrice Jollant, MD, PhD, professor of psychiatry, University of Paris, France, told Medscape Medical News.
Swift, Full Remission
The study included 156 adults admitted voluntarily to seven French teaching hospitals with severe suicidal ideation, including 52 with bipolar disorder, 56 with depressive disorder, and 48 with other psychiatric diagnoses…… “We investigated the full remission of suicidal ideas and not only the response, which is usually defined as a reduction of 50% of scores on a given scale. If people remain slightly suicidal, the suicide risk persists. We want all suicidal ideas to disappear,” said Jollant. They found that more patients reached full remission of suicidal ideas at day 3 after two ketamine infusions than after placebo infusions …………. This anti-suicidal effect of ketamine was rapid, with 44% remission only 2 hours after the first infusion, the authors report. The effect of ketamine on suicidal remission was greatest in patients with bipolar disorder, with 85% achieving full remission at day 3. At 6 weeks after treatment, remission in the ketamine group remained high, ………
Ketamine might therefore exert its effects through analgesic mechanisms that reduce mental pain,” they write.
Ketamine’s side effects were “limited” with NO manic or psychotic symptoms seen. The main side effects, including sedation, denationalization/derealization, nausea, and dizziness, were of short duration and occurred in about 10% or fewer patients……..
it shows that another important group of patients with acute suicidal ideation, those with bipolar disorder, could benefit from ketamine,” De Giorgi writes.
Ketamine vs ECT “Shock Therapy” Electroconvulsive Therapy (ECT) Electroconvulsive Therapy (ECT) is the gold standard treatment for treatment Resistant Depression, but results of a new randomized, head-to-head trial suggest intravenous Ketamine is at least as effective as ECT “Shock Therapy and has fewer side effects.
“The take-home message right now is that if somebody is being referred for ECT [“shock therapy”], the treating clinician should think of offering ketamine first,” study investigator Amit Anand, MD, professor of psychiatry, Harvard Medical School, Boston, Massachusetts, told Medscape Medical News.
The study was published online May 24 in The New England Journal of Medicine. More than one-third of cases of depression are treatment resistant, said Dr. Anand, who is also director of Psychiatry Translational Clinical Trials at Mass General Brigham. He noted that ECT [“shock therapy”], has been the “gold standard for treating severe depression for over 80 years.” He added that although ECT [“shock therapy”], is very effective and is fast acting, “it requires anesthesia, can be socially stigmatizing, and is associated with memory problems following the treatment.” An anesthetic agent, ketamine has been shown to have rapid antidepressant effects and does not cause memory loss or carry the stigma associated with ECT, he added.
For these reasons, the investigators examined whether it may be a viable alternative to ECT [“shock therapy”].
To date, no large, head-to-head trials have compared ECT [“shock therapy”], to intravenous ketamine. A recent meta-analysis showed that ECT was superior to ketamine for major depression, but the total number of patients included in the analysis was small, Anand said. In addition, most of the participants in that trial were drawn from a single center. Approximately 95 patients were enrolled in each arm of the trial, which included some participants with features of psychosis. “ECT is very effective for depression associated with psychotic features, which may be one reason ECT had a better response in that trial,” said Anand. The investigators compared ECT to ketamine in a larger sample that excluded patients with psychosis. They randomly assigned 403 patients at five clinical sites in a 1:1 ratio to receive either ketamine or ECT (n = 200 and 203, respectively; 53% and 49.3% women, respectively; aged 45.6 ± 14.8 and 47.1 ± 14.1 years, respectively). Patients were required to have had an unsatisfactory response to two or more adequate trials of antidepressant treatment. Prior to initiation of the assigned treatment, 38 patients withdrew, leaving 195 in the ketamine group and 170 in the ECT group. Treatment was administered over a 3-week period, during which patients received either ECT three times per week or ketamine twice per week. The primary outcome was treatment response, defined as a decrease of ≥50% from baseline in the 16-item Quick Inventory of Depressive Symptomatology-Self-report (QIDS-SR-16). Secondary outcomes included scores on memory tests and patient-reported quality of life. Patients who had a response were followed for 6 months after the initial treatment phase. …………………
“ECT [“shock therapy”], was associated with musculoskeletal adverse events,
whereas ketamine was associated with dissociation,” the investigators note. ECT [“shock therapy”], has been shown to be effective for older adults, patients with MDD and psychosis, and in inpatient and research settings. Future studies are needed to determine the comparative effectiveness of ketamine in these populations, the authors note.
Commenting for Medscape Medical News,
Dan Iosifescu, MD, professor of psychiatry, at NYU Grossman School of Medicine, New York, called it an “extraordinarily important and clinically relevant study, large, well-designed, and well-conducted.”The main point of this study is that the two treatments are largely equivalent, although numerically, ketamine was slightly associated with more beneficial outcomes and fewer cognitive side effects,” he said.
The findings suggest “that people who have no contraindications and are candidates for both ketamine and ECT — which is the vast majority of people with treatment-resistant depression — should consider getting ketamine first because it is somewhat easier in terms of side effects and logistics and consider ECT afterward if the ketamine doesn’t work.”……….
Kentuckiana Ketamine Institute looks forward to helping individuals with the above-described challenges.